I Broke My Wrist: My Journey Through Distal Radius Fracture Recovery
On Saturday, May 25th, 2024, I was doing something I'd done almost every other weekend for the last two years: riding a scooter (a typical two wheel scooter, no motor) right behind my five-year-old son (while he rides his bike). But that day turned out differently. I lost my balance, had a bad fall, and landed on my left wrist. I knew instantly something was wrong because my wrist was in an abnormal position. Fortunately, my son was okay. We were right next to my house, so my partner came over, and I went to the ER. An x-ray revealed I had fractured my distal radius (the top of the bigger bone in the forearm, right at the wrist). I had surgery 4 days later (May 29th).
This post reflects on my experience to provide perspective for those who might be going through something similar.
Diagnosis
At the hospital, I was given an x-ray, which showed a fracture. I was put in a splint and scheduled for an appointment on Tuesday (Monday was Memorial day, so public holiday), two days after the fall. I was prescribed pain medication and put in an finger-elbow splint to immobilize my arm from the elbow down to my fingertips. I almost forgot to mention, the pain after the fall was excruciating - especially the 3 days after.

Diagnosis: Distal Radius Fracture, Volar Type, Articular Involvement, Displacement
The distal radius is the end portion of the radius bone near the wrist. A distal radius fracture occurs when this part of the bone breaks. The volar type fracture specifically refers to a fracture where the break is on the volar side (the palm side) of the wrist. The volar (or palmar) side is the side of the forearm and wrist that faces inward, towards the palm. Fractures on this side can be more challenging because of the important tendons, nerves, and blood vessels that run along this path. I also had some displacement, which means the bones were not aligned correctly. Finally, articular involvement means that the fracture extends into the joint surface of the wrist. This can be more complicated because it can affect the joint surface and the cartilage that helps the bones move smoothly.
When I got the x-ray, the doctor frowned and said it was a bad break. I didn't really understand what that meant at the time, but I later did after some research (described above).
Making a Decision, Fast
When I met with the orthopedic specialist, I learned a few things. First, most fractures (and given my age .. 37 at the time) will heal naturally in a 3-6 week period. However, if the bones do not heal in the right position, there could be long-term pain, potential arthritis, and other issues. Surgery (ORIF) was recommended to realign the bones and hold them in place with hardware like a metal plate and screws.
ORIF stands for open reduction and internal fixation. ORIF wrist surgery, or open surgery for wrist fractures, is a technique used to reposition, stabilize and heal a severely broken wrist. Internal fixation means hardware such as pins, screws, or wires is used to hold the broken bones together. This most often occurs in a distal radius fracture; fractures involving the lower portion of the radius, the larger bone of the forearm.
I made this decision in a relatively short time and it was hard. For anyone in a similar situation, this will be a challenging decision - it certainly was for me. In my case, given the displacement and multiple fracture parts (creating risks of displacement during healing if not fixed), I opted for surgery. I would later learn that having a metal plate significantly reduces recovery time, especially the amount of time spent in hard immobilizing/stabilizing splint. Also, the longer a body part is immobilized, the longer it takes to regain range of motion and strength.
The surgery was scheduled for the next day (4 days after the fall).
Surgery
This was my first major surgery, aside from a wisdom tooth removal three years prior. The preparation involved a lot of questions about my health, habits, and allergies. I received an overview of what would happen, including how anesthesia works and its post-operative effects. After being wheeled into the operating room, I awoke in the recovery room. I had a splint with a hard shell on the bottom of my hand (where the surgery incision was made). The screws and metal plate prevent further displacement and act to hold the bones in place while they heal. I was told that the surgery went well, and I was discharged the same day with a prescription for pain medication and a follow-up appointment in a week.
I felt very woozy and seem to be missing chunks of memory from that day (e.g., things the doctor told me post surgery, conversations I had). Conversations with my wife and son on the ride home felt like they were in slow motion—a very foggy and unusual experience. I was told that these were some expected anesthesia effects. I surprisingly still had a mild version of this foggy effect a week after surgery (like I am in a conversation and can’t think clearly).
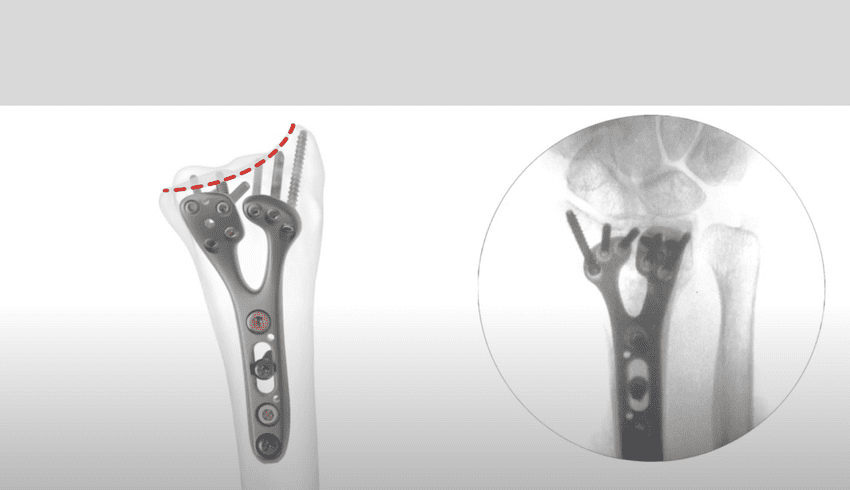
Terminator jokes aside, I now have a titanium plate and screws in my left forearm. And I asked all the natural questions - will I set off metal detectors at airports? Do the screws have to be removed? Can I lift weights again? The answers were: no (usually), no (unless they cause issues), and yes (eventually, but not for a while).
Pain and Discomfort
I have a fairly high pain tolerance, but I had also prepared myself mentally for the pain. I had pain medication and numbing medicine from the hospital post surgery, which made my entire hand numb, leading to a burning sensation in the first two days. This discomfort would wake me occasionally, and I spent those times trying to get my fingers moving. I took the prescribed extra strength advil as needed over the first 3 days. I never took the prescribed narcotics but was grateful to have them on standby.
Feelings
From the moment the accident happened, I experienced many emotions. I was terrified about the potential long-term effects: permanent pain, loss of strength, and a long recovery time. Will I have issues down the road with a permanent titanium plate in my forearm? I had read that regaining range of motion could take up to three months, typing up to six months, and full functionality (e.g., pushups) up to a year. Additionally, I had several important family events planned months in advance, had many activities I really enjoy that require two hands (dont we all?) and I did not know how to manage all of it. As a computer scientist, the thought of not being able to type for six months was extremely scary.
Finding the Silver Lining - Making a Plan**
I've had setbacks in the past, and I've learned that how you handle them influences the outcome. When life gives you so called lemons, make lemonade. So, I started planning. Here are a few things I did:
- Take Time Off Work: I knew I needed to focus on my recovery and have the psychological space of a full disconnect. It can be tempting to muscle through, work part time etc. I just knew that this was not one of those times. I was fortunate to have a supportive work environment that allowed me to take time off.
- Family Time: I decided I'd use this experience as an opportunity connect more with my son and support my partner. Let them be there for me and let them know that I was there for them. I had an injured hand, but there are many other things you can do (even if slowly). I couldn’t drive for a while, but I take on some house work, dishes, laundry, mail, story time and other things for my son etc.
- Invest in Recovery: I knew that recovery speed, strength, and range of motion were highly correlated with the amount of therapy and exercise put into it. I spent hours going through finger motions pushing through the initial pain.
Recovery
I was surprised at how quickly my fingers forgot how to move. The injury and surgery caused inflammation and stiffness, so my muscles had to relearn basic functionalities. Very fast, I realized there seemed to be three main components in my recovery:
- Bone Healing: This was mostly out of my control, dependent on time and genetics.
- Range of Motion and Strength: This required much work to overcome the stiffness and build muscle memory.
- Long-term Pain and Nerve Damage: This scared me the most, but I focused on what I could control.
With these realizations, my focus was on #2 - pushing through the pain to regain range of motion and strength - pretty much the only thing I could control.
Daily Progress
-
Day 1: I couldn't touch my index finger to my thumb, but I could form a light hook/claw and an L position. More like my hand was in a permanent claw position and it took a lot of pain with trembling to attempt barley opening it.
-
**Day 2:**By day 2 the numbness in my had had started to wear off a bit more, I better judged my pain levels and started more exercises. I could pick up light objects (like paper 😊) and touch my index finger to my thumb.
-
Day 3: I could touch my thumb to my index, middle, and ring fingers lightly. Significant progress already!
-
Day 4: I did a typing test: 45 WPM with 96% accuracy. I could perhaps type for 5-10 mins before it got too painful/uncomfortable. I intend to use this as a baseline to track progress.
-
Day 5: I tied my shoelaces (very lightly/gingerly). Still working through finger stretches, there is still quite a bit of pain.
-
Day 6: First post operation doctors visit. Bandages changed, still a semi-hard cast (hard on surgery surface). Follow-up x-rays showed some suspected ligament damage. This was a really low day as this has been one of my biggest fears. It is still suspected and only time will really tell what needs to be done. I was instructed to focus on finger movements and making a fist as opposed to any wrist movement (pronation, supination, flexion or extension).
-
Day 10: Swelling and inflammation had greatly reduced. I didn’t need to elevate my hand all day, but I still felt occasional numbness especially after waking up each morning.
-
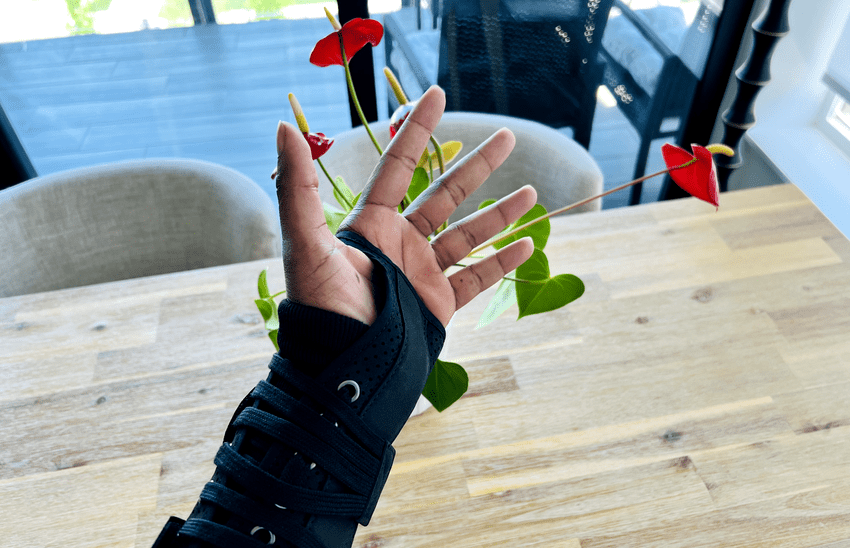
Day 13: Second post operation doctors visit. Stitches removed. Now in a velcro removable brace (screenshot above). Very emotional day - seeing my scar, reflecting on what the journey ahead could look like. Grateful for and proud of the recovery I had made so far. Was told that I had really good range of motion and progress given the time since surgery. There are still motions are are extremely painful (like trying to make a fist, now that I have a thinner brace) but I am told that is normal. Physical therapy starts the following week.
-
Day 216 (7 months post surgery): I can now do pushups, pullups exercises at about pre-surgery level. However, I still feel some pain in my wrist after any of these sessions (especially load bearing activities like puhsups) so I tend to do those types of exercises very sparingly. Flexion, extension, pronation and supination are about 95% of pre-surgery level.
Conclusion
There's no profound revelation here, just another data point for anyone going through a similar experience. This journey was jolting, but it too shall pass.
Lessons Learned
- Health: I realized my body isn’t as strong as it used to be, and I need to invest more in my health and exercise. Would the fracture have been avoided if I was in better physical conditioning? I don't know. What I know is that I want to give myself any advantage, especially as I get older.
- Family: This experience reminded me of what matters most: my family and loving the people around me.
- Gratitude: I’m incredibly thankful for my supportive work environment and my understanding manager.
- Individual Journeys: Everyone’s recovery journey is different, and that’s okay. Your own recovery journey may be shorter, longer, easier or harder than what I have above. And that's okey.
Thank you for reading, and to anyone going through something similar, know that it gets better.
 2020 Year in Review
2020 Year in Review Research Internship -- So It Begins.
Research Internship -- So It Begins. Why I moved my personal website to Gatsby.js + Github
Why I moved my personal website to Gatsby.js + Github Hello World VR Application with the Oculus Quest 2 and Unity
Hello World VR Application with the Oculus Quest 2 and Unity 2022 Year in Review
2022 Year in Review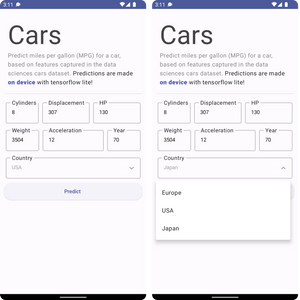 How to Build An Android App and Integrate Tensorflow ML Models
How to Build An Android App and Integrate Tensorflow ML Models